HPTA Restart Protocol for Discontinuing TRT (2020)
Jasen Bruce
May 18, 2020

The volume of testosterone prescriptions continues to rise in the US as more evidence emerges supporting the tremendous benefit of testosterone therapies in aging men.
One unfortunate result of the increase in testosterone prescriptions has been men who have been misdiagnosed with low testosterone but still placed on testosterone replacement therapy (TRT) when it may not have been needed in the first place. In other cases, men chose to self-medicate with androgenic and anabolic hormones without being properly monitored.
If you are one of these men and you are considering the discontinuation of testosterone treatments, there is a protocol that can help prevent hormone withdrawal symptoms by quickly restoring your own hormone production.
Discontinuing testosterone abruptly can lead to avoidable discomfort and side effects that can be mitigated with proper intervention. Learn more about the potential symptoms you could experience if you quit TRT cold turkey.
Fortunately, there is enough evidence available to guide experienced physicians who prescribe personalized protocols that are designed to help patients recover their own endocrine system.
Before getting started, it's important to give your physician a detailed history. This history should include:
- Previous hormone use
- Type of hormones used
- Dosage form
- Duration of use
Your doctor should also review any laboratory tests, along with a general health evaluation to address conditions and other factors that might influence endocrine health.
What is the HPTA Axis, and What Does it Mean to Restart It?
Men who have been taking testosterone or similar androgens for a long period of time (more than four weeks) may experience secondary hypogonadism produced by the negative feedback response to the testosterone supplementation.
This results in the body slowing down or stopping its own production of testosterone.
Sometimes the body does not recover quickly enough on its own, leading to a reduced quality of life and symptoms related to low testosterone.
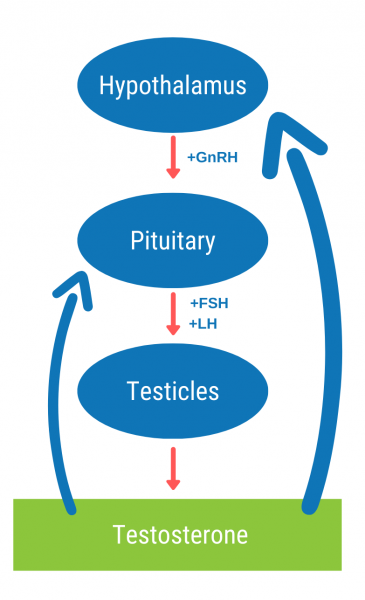
Natural testosterone production relies on a balance of hypothalamus hormones including gonadotropin releasing hormone (GnRH), pituitary hormones including luteinizing hormone (LH), and the testicles where testosterone is produced. This is called the Hypothalamus-Pituitary-Testicular axis, or HPTA.
When the body recognizes elevated hormones in the blood, it prevents the pituitary from releasing LH, and without stimulation from LH, the testicles are unable to produce testosterone.
This is not a problem in men who are supplementing testosterone (TRT), but once the hormone is discontinued, there is nothing to replace it. The result is hormone withdrawal symptoms.
HPTA Restart Protocol for Men Discontinuing TRT
Most common protocols used to restart natural testosterone production utilize a combination of hormone stimulators designed to address the different areas affected by negative feedback.
This includes the stimulation of LH production in the pituitary or stimulation of the testicular cells to produce testosterone.
Sometimes, a combination protocol is prescribed to first increase testicular volume and testosterone production using a gonadotropin like HCG, followed by pituitary stimulation to increase LH production using a class of medications known as selective estrogen receptor modulators (SERMS). Since HCG mimics LH, the goal is for the body’s LH to take over communicating with the testicles to maintain volume and adequate testosterone production.
There may be cases where a patient cannot maintain adequate testosterone production on their own after discontinuing hormone supplementation. The HPTA restart protocols can also be used as a diagnostic tool to help the physician determine where the body is failing to support natural testosterone production, and if testosterone replacement therapy is needed.
Common Medications used for HPTA Restart
Physicians will typically use one or more of these medications in a personalized regimen that considers the patients previous hormone use, current condition, and other factors assessed during the appointment. This list is not all-inclusive, since there are similar medications sometimes used by specialists depending on their experience with the drug and their goals for the patient.
- Human Chorionic Gonadotropin (HCG)
- Clomiphene citrate capsules or tablets
- Tamoxifen citrate capsules or tablets
- Toremifene citrate tablets
- Low dose anastrozole, sometimes used
- Follicle Stimulating Hormone (FSH) is sometimes used with HCG to improve fertility and testicular function
- PDE5 inhibitor like tadalafil or sildenafil to treat erectile dysfunction
When to Start Therapy
When discontinuing a long-acting injectable ester, such as cypionate or enanthate, therapy to stop TRT is usually initiated roughly five days after the last injection, as the hormone levels start to fall.
For faster-acting dosage forms like topical creams and suspensions, HPTA treatment should typically be initiated one day after administering the last dose.
Patients discontinuing hormone pellet therapies need to wait at least two months after insertion before hormone levels begin to fall.
Many progressive testosterone physicians prescribe HCG for men to take during testosterone replacement therapy to help maintain testicular volume and fertility. Using HCG during hormone supplementation can help the HPTA recover faster after hormones are discontinued.
Blood Work for Discontinuing TRT
Laboratory tests are used to determine the effectiveness of the treatment, because they allow the physician to look at hormone levels. Certain hormones should be responding to treatment, and if they are not responding, adjustments can be made to the protocol.
Some of the hormone and metabolic markers tested include:
- Testosterone free and total
- Estradiol (sensitive)
- Luteinizing hormone (LH)
- CBC
- CMP
- Lipids
Results-Driven Protocols for Stopping TRT
Patient success is measured by how they respond to treatment. The goal is to restore endogenous (natural) hormone production to adequate levels and alleviate any negative symptoms that affect quality of life.
In rare cases, someone may not be able to produce hormones on their own. This is called primary hypogonadism and results from the testicles’ inability to respond to LH (or HCG) stimulation. This in turn results in low testosterone production. Patients diagnosed with primary hypogonadism can benefit from testosterone replacement therapy managed by an experienced physician.
The result is relief of symptoms and improvement of metabolic and endocrine health.
If you want to discontinue hormone therapy or self-medicating hormones, contact Defy Medical to connect with an experienced care team that knows how to manage your hormones.
*This article is intended to provide general information for these considering making a change. For best results, schedule a consultation with an experienced practitioner to discuss your individual health and goals to determine the most effective protocol for you.
References
- Wheeler KM, Sharma D, Kavoussi PK, et al. Clomiphene citrate for the treatment of hypogonadism. Sex Med Rev 2019;7:272–276
- Madhusoodanan V, Patel P, Lima TFN, et al. Human Chorionic Gonadotropin monotherapy for the treatment of hypogonadal symptoms in men with total testosterone > 300 ng/dL. Int Braz J Urol. 2019;45(5):1008‐ doi:10.1590/S1677-5538.IBJU.2019.0132
- Rambhatla A, Mills JN, Rajfer J. The Role of Estrogen Modulators in Male Hypogonadism and Infertility. Rev Urol. 2016;18(2):66‐ doi:10.3909/riu0711
- Rodriguez KM, Pastuszak AW, Lipshultz LI. Enclomiphene citrate for the treatment of secondary male hypogonadism. Expert Opin Pharmacother. 2016;17(11):1561‐ doi:10.1080/14656566.2016.1204294
- McBride JA, Coward RM. Recovery of spermatogenesis following testosterone replacement therapy or anabolic-androgenic steroid use. Asian J Androl. 2016;18(3):373‐ doi:10.4103/1008-682X.173938
- Kohn TP, Louis MR, Pickett SM, et al. Age and duration of testosterone therapy predict time to return of sperm count after human chorionic gonadotropin therapy. Fertil Steril. 2017;107(2):351‐e1. doi:10.1016/j.fertnstert.2016.10.004
- El Osta R, Almont T, Diligent C, Hubert N, Eschwège P, Hubert J. Anabolic steroids abuse and male infertility. Basic Clin Androl. 2016;26:2. Published 2016 Feb 6. doi:10.1186/s12610-016-0029-4
- Kanayama G, Hudson JI, DeLuca J, et al. Prolonged hypogonadism in males following withdrawal from anabolic-androgenic steroids: an under-recognized problem. Addiction. 2015;110(5):823‐ doi:10.1111/add.12850